What is a Joint Cartilage and Why is it Important in the Body?

In every moving part of your body, there’s a connective tissue whose role is to serve as a cushion between the bone and the joint. The role of this flexible fibrous tissue in the body is incredibly important as it protects moving bones from touching the joint and essentially causing the stiff, painful feeling.
The human body has three types of cartilages, namely; Elastic cartilage, Fibrocartilage and Hyaline cartilage and they all have distinct features. Of importance is the joint cartilage, – a unique tissue of diarthrodial joint whose absence automatically results in arthritis. If it is damaged, however, lots of details and procedures would go into ensuring it heals and functions well.
But, what exactly is a Joint Cartilage?
As the basic science of Articular Cartilage explains, this super-tough and flexible material acts as a cushion between the joint and the bones. However, this joint cartilage is officially referred to as articular cartilage for it covers the entire surface where the articulate born meets the joint. Basically, it is the cartilage found at the knee joint and whose main role is to ensure no friction is generated as the femur or the tibia glide over the joint.
What it’s made of
This cartilage type primarily consists of type II collagen as well as chondroitin sulfate; two components that also make up the elastic cartilage as well. The largest share of the components that form its cartilage is known as hyaline cartilage. However, to augment its two main purposes of absorbing shock and enabling smooth movements, this smooth, rubbery connective tissue has what’s known as synovial fluid as well.
Much as all joint cartilages in the body specifically serve the same purpose, it is their locations and thicknesses that differ. At the knee joint, for example, the articular cartilage is understandably thicker by 6mm or so, unlike that of the wrist which may be 1mm or less. With the sticky, viscous synovial fluid lubricating the joint, however, any movement becomes a lot easy and painless.
Important to note:
There are two facts to bear in mind regarding the articular cartilage. They are:
1.Functions of the articulate cartilage
First, its major purpose is to allow smooth, trouble-free movements between the joint and the bones surrounding it. The way it enables this is quite simple; the bones glide over the soft cartilage tissue and the friction created is lubricated by the special synovial fluid.
Aside from that, joint cartilages serve an all-important purpose of absorbing all the shock generated during mobility. The soft tissue prevents the joint from rubbing and crushing against each other under the body’s heavy mass, especially when you are walking or jogging.
2. Joint cartilage doesn’t heal
Another vital fact has to do with any damages suffered by the articulate cartilage. With time, the thickness of this tough tissue reduces, essentially due to years of constant usage. Whether it’s the normal wear and tear or it’s due to a disorder, its size gradually reduces.
When the size of the cartilage reduces, a person tends to feel some kind of pain and stiffness on the affected joint. Collagen fibers, proteoglycan, and elastin that form this tissue have no blood vessels and thus can’t get any nutrients for their growth and regeneration. And so, any damage on them or when they begin to age, the process will continue until it eventually becomes arthritis.
Cartilage Restoration
Regardless of its strength and usefulness, joint cartilage can suffer immense damage. Three of the most notorious causes of damages suffered by this cartilage are:
• Injuries
• Normal wear and tear that often leads to Osteoarthritis
• Common conditions like Rheumatoid Arthritis and Ankylosing Spondylitis.
Articulate cartilages have no nerves and so, when it gets damaged, no pain is felt. However, that does not mean you will still walk around with ease, like before.
When it is damaged, the joint will inherently suffer the brunt from the bones. The bones will rub against it, resulting in friction and abnormalities like bone spurs. It isn’t a feeling you would fancy experiencing because it can cause lots of pain and discomfort.
How to Rectify a Damaged Articulate Cartilage
Once it gets damaged, the cartilage will never grow and recover back to its original form. And while medics have been trying out several surgical techniques meant to initiate a fresh growth of the cartilage, restoration procedures still vary.
1. Identification of the Damaged Cartilage
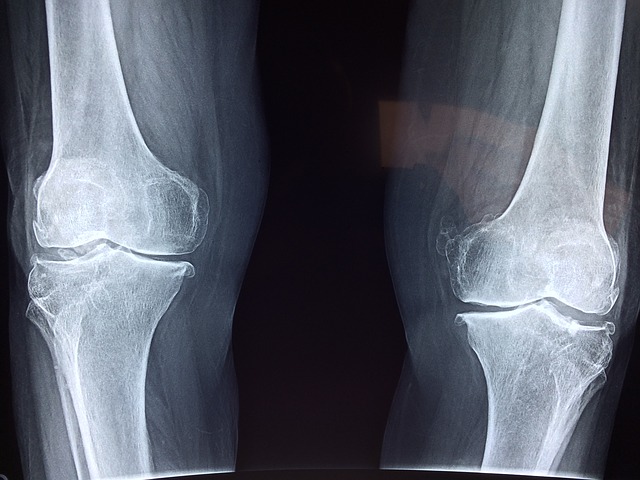
It is normal for a patient diagnosed with either meniscal injury or ligament tears to have also suffered cartilage damage. Establishing the extent of damage isn’t easy though given that the majority hyaline cartilage can’t be detected via X-ray. The doctor, therefore, recommends surgery on the affected joint.
2. Not everyone goes under the knife
Articulate cartilage is pretty delicate and not everyone is recommended to undergo a surgical procedure. Essentially, young adults are admitted without lots of questions, unlike senior patients whose health can be jeopardized by the procedure.
Away from eligibility, however, a single injury (a lesion) can be operated on. The commonest joint for cartilage restoration is the knee joint. Ankle and shoulder are acceptable for this treatment method too.
3. Common cartilage restoration procedures are:
Most of the surgical procedures are performed arthroscopically, whereby the surgeon targets the joint area and makes some tiny puncture incisions – three of them. The main reason for this style of surgery is because it is not as painful as the conventional method and recovery take a shorter period.
However, the various surgical procedures done arthroscopically are:
Microfracture
This procedure basically involves pumping fresh blood to encourage the growth of new cartilage on the area operated on. The best candidates for microfracture, however, are those whose subchondral bones are healthy and have single lesions.
Drilling
It is another style of triggering the growth of healthy cartilage whereby the subchondral bone is drilled using a surgical drill. No blood is pumped into the multiple holes made, although the problem with this method is the fact that it’s less precise and can potentially damage other tissues.
Abrasion Arthroplasty
It’s almost analogous to drilling, only that the procedure involves high-speed burrs as an alternative to drilling. It is also done using an arthroscope.
Autologous Chondrocyte Implantation
This is a unique, 2-step method of treating damaged cartilage. Basically, new cartilage is regenerated, a process that takes 3-5 weeks. When the new cartilage matures, it is implanted on the damaged area. This method mostly appeals to younger patients.
Two other procedures are Osteochondral Autograft Transplantation and Osteochondral Allograft Transplantation. The former involves transplanting healthy cartilage from a joint to the damaged one.
If the damage is massive in size, an Osteochondral Allograft Transplantation procedure will be done. This will basically involve getting a tissue graft from a cadaver donor, resizing it and implanting on the damaged joint.
4. Rehabilitation
After undergoing any of the above methods, the patient will have to protect the area operated on so that the cartilage heals well. Rehabilitation is a series of processes and can involve physical therapy among other activities. In the end, the joint cartilage heals well enough to allow a person to resume a normal life.
